Acquired Peripheral Retinoschisis
Acquired Peripheral Retinoschisis
INITIAL PRESENTATION
Chief Complaint
Persistent floaters and decreased nasal visual field in right eye
History of Present Illness
An 83-year-old male was referred to our retina clinic for a retinal detachment which was described as close to the macula in his right eye. He was asymptomatic on presentation. He reported a 2-year history of floaters and noted decreased nasal visual field in his right eye for several years. The patient previously worked as a welder and had a history of metallic corneal foreign bodies but had not experienced any recent trauma. He denied photopsias and had no family history of retinal detachments.
Past Ocular History
- Ocular hypertension
- Metallic corneal foreign bodies
- No previous eye surgeries
Past Medical History
- Coronary artery disease status post carotid endarterectomy
- Myocardial infarction status post heart stent placement
- Hypertension
- Hyperlipidemia
Past Surgical History
Medications
- Timolol twice daily in both eyes
Allergies
Family History
- No history of retinal detachment
Social History
Review of Systems
- Negative except as listed in history of present illness
OCULAR EXAMINATION
Visual Acuity without correction
- Right eye (OD): 20/20 -3
- Left eye (OS): 20/40; pinhole: 20/30 -2
Ocular Motility
Intraocular Pressure (IOP)
Pupils
- Pharmacologically dilated at arrival so unable to test for afferent pupillary defect
Confrontation visual fields
- OD: Partial superior temporal, inferior temporal deficiencies
- OD: Full field
Slit lamp exam
OU
- External/Eyelid: Normal
- Conjunctiva/Sclera: Clear and quiet
- Cornea: Clear
- Anterior chamber: Deep and quiet
- Iris: Normal architecture
- Lens: 2+ nuclear sclerosis, 1+ posterior subcapsular cataract
Dilated fundus examination (DFE)
OD
- Vitreous: No posterior vitreous detachment (PVD), no heme or pigment, no vitreous cells
- Disc: normal
- Cup to disc ratio: 0.2
- Periphery: Temporal retinoschisis from 7:00 to 10:00 without identified inner, outer, or full-thickness breaks; inferior edge adjacent to area of chorioretinal atrophy. There is an absolute visual field deficit through the entire area.

Figure 1a: (OD) Fundus photo showing temporal retinoschisis from 7:00 to 10:00 without identified inner, outer, or full-thickness retinal breaks extending into the temporal macula.

Figure 1b: Here is an additional picture of a different patient showing inferotemporal retinoschisis
OS
- Vitreous: No PVD, no heme or pigment, no vitreous cells
- Disc: normal
- Cup to disc ratio: 0.2
- Periphery shows a faint shallow retinoschisis inferotemporally for 4-5 clock hours, much less bullous compared to the right eye
DIFFERENTIAL DIAGNOSIS
CLINICAL COURSE
The patient underwent an uncomplicated clinical course. No ophthalmologic intervention was necessary. Signs and symptoms of retinal detachment were reviewed and he was provided with reassurance.
DIAGNOSIS
Acquired retinoschisis
Diagnostic Criteria[1]
- Elevation of the inner layers of the neurosensory retina due to microcystoid degeneration. The lesion appears relatively immobile, transparent, smooth-domed and bullous in appearance.
- Minimal pigment alterations or atrophy of the retinal pigment epithelium layer
DISCUSSION
Definition
Retinoschisis (RS) literally means "a split in the neurosensory retina"[2]. Acquired retinoschisis, also known as degenerative or senile retinoschisis, is an acquired, idiopathic condition characterized by gradual, peripheral splitting of retinal layers. This produces a well-circumscribed, transparent dome-shaped elevation of the inner retina that extends anteriorly towards the ora serrata[3]. Two histological forms, typical and reticular, have been previously described[4].
Typical retinoschisis[4]
- Appearance: a bubbly, round appearance best visualized with scleral depression; the retinal splitting typically extends 2-3mm posterior to the ora
- Etiology: the retina splits in the outer plexiform layer, allowing the visualization of the footplates of the Muller cells, seen as white dots
- Complications: it is very uncommon for the retinal splitting to extend posteriorly towards the macula or form outer layer holes. Thus the risk for retinal detachment is lower than that of the reticular subtype
Reticular retinoschisis
- Appearance: an oval shaped, bullous elevation with a finely stippled internal surface and sclerotic looking retinal vessels; typically located posterior to and continuous with typical peripheral cystoid degeneration
- Etiology: the retina splits in the nerve fiber layer, similar to Juvenile X linked retinoschisis
- Complications: retinal holes in the outer wall occur in 23% of cases; posterior extension toward the macula is more common when compared to the typical subtype[5].
Epidemiology
- Reported prevalence of disease varies widely due to population-based RS studies, difficulty of observing lesions due to its peripheral location, and the fact that most patients are asymptomatic. Some studies have demonstrated prevalence rates of 3.9% (95% confidence interval, 2.6–5.2) in persons aged 60 to 80 years old[6]. In a previously reported case series, incidence of retinoschisis was found to be 3.7% in patients 10 years or older and 7% for patients 40 years of age or older, with 82% of cases being bilateral[7]. Men and women from all ethnicities seem to be affected equally[6]. RS lesions are most commonly found in the inferotemporal quadrant of the peripheral retina[5 ,8].
Clinical Features
Signs and Symptoms
- RS rarely produces symptoms in the absence of a retinal detachment and is typically found on routine dilated fundoscopic exam[9] .
Exam, Testing and Imaging
- Diagnosis is typically based on ophthalmoscopy with scleral depression and contact lens examination (Figure 2), although lately optical coherence tomography (OCT) has been shown to play a significant role in distinguishing acquired RS from retinal detachment[2]. OCT can be used to obtain detailed cross-sectional images of the peripheral retina (Figure 3)[1].
- OCT: The schisis occurs at the junction between the outer plexiform layer and inner nuclear layer of the neurosensory retina in the typical subtype[2].
- Fundoscopy: RS appears as an immobile, dome-shaped elevation of the retina[10]. The height of the schisis cavity will not shallow with scleral indentation[2].
- Visual Field Testing: an absolute visual field defect will be present in the affected area. However, since RS typically occurs anterior to the equator in the periphery of the retina, typically no visual field defect is detected[9].
Clinical Feature |
Retinal Detachment |
Retinoschisis |
Surface: |
Corrugated (unless chronic) |
Smooth, domed |
Hemorrhage or Pigment: |
Present |
Absent |
Scotoma: |
Relative |
Absolute |
Reaction to Laser: |
Absent |
Generally Present |
Shifting fluid: |
Variable |
Absent |
Table 1: Distinguishing clinical features of Retinal Detachment and Retinoschisis
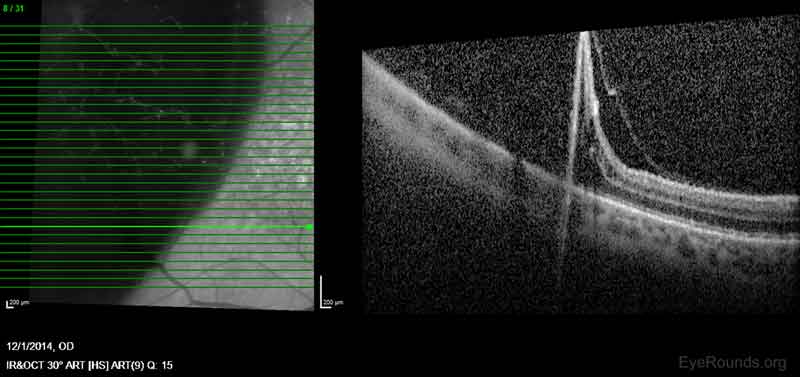
Figure 2: OCT image showing separation of the retina in the outer plexiform layer
Etiology and Pathogenesis
Although the exact etiology is unknown, there is no evidence to suggest a genetic, vascular, or nutritional etiologic component[3]. The degenerative (acquired) form of RS is believed to progress from preexisting peripheral cystoid degeneration in the retina[5]. The existing cystic lesions essentially fuse together as neuroretinal and glial supporting elements within each lesion degenerate. This area slowly enlarges over time resulting in separation of the retina into an inner and outer layer. As the retina continues to split, neurons in that area are disrupted, causing irreversible and complete loss of visual function in the affected area[3 ,11].
Management and Treatment
Various treatment and management strategies are continually under debate as degenerative RS has been found to be primarily asymptomatic and non-progressive[8]. Most cases of retinoschisis are innocuous and do not affect central vision. Frequency of the follow up visits depends upon the lesion size, its proximity to the macula and the presence or absence of symptoms (6-24 month intervals). Patients should be advised to return urgently if they experience symptoms of retinal detachment. Treatment (laser surgery, incisional surgery) should be considered only in symptomatic cases that threaten the macula and in cases with progressive retinal detachment[8]. Although retinal detachment due to underlying RS can occur, unless the retinal detachment is full thickness, it is possible for patients to maintain good vision without surgical intervention. This is true even with foveal involvement in some cases[12] (Table 2).
Stage of senile retinoschisis |
Treatment |
without retinal breaks |
no treatment (except rarely) |
with outer-layer retinal breaks |
no treatment (except rarely) |
with localized 'schisis-detachment' |
no treatment (except rarely) |
with progressive, symptomatic RD |
prompt surgical repair |
Table 2: Treatment options for Degenerative Retinoschisis based on severity of disease[10]
Complications
The rate of RS progression to symptomatic retinal detachment is estimated to be between 0.05% and 2.2%[6 ,8]. However, this progression is responsible for roughly 3% of full retinal detachments overall. It has been shown that those with a family history of retinal detachment have an increased risk of this complication[5]. The presence of retinal holes is related to the two types of retinal detachments that are possible from progression of RS. RS without retinal breaks in either layer will never lead to a retinal detachment[3]. Retinal holes may be seen in the outer or inner retinal layer of RS lesions, however, outer holes are much more common[8]. Outer layer retinal holes (Figure 5) may exist with or without a co-exisitng RD [11]. If a retinal detachment is present, it is localized and fairly stable (non-progressive). Outer retinal holes in isolation are more common compared to outer + inner layer holes[3]. Outer and inner retinal layer holes are associated with symptomatic, rapidly progressive retinal detachments. This scenario allows for collapse and quick progression into a full thickness rhegmatogenous retinal detachment that requires urgent surgical treatment. These dual layer holes are a rare occurrence in patients with RS who are initially asymptomatic[3]. Treatment with laser demarcation or more invasive surgical intervention would be similar to treatment of conventional retinal tears or detachments[5 ,13].

Figure 3: Outer retinal holes in the setting of superotemporal retinoschisis.
SUMMARY
EPIDEMIOLOGY
- Found in ~4% of population
- ~30% of affected individuals have bilateral involvement
|
SIGNS
- Often an incidental finding
- Absolute scotoma
|
SYMPTOMS
- Asymptomatic usually
- Scotoma
|
TREATMENT
- Observation, 3% risk of retinal detachment
|
References
- Stehouwer M, Tan SH, van Leeuwen TG, Verbraak FD. Senile retinoschisis versus retinal detachment, the additional value of peripheral retinal OCT scans (SL SCAN-1, Topcon). Acta Ophthalmol 2014;92(3):221-227. [PMID 23773202]
- Yeoh J, Rahman W, Chen FK, da Cruz L. Use of spectral-domain optical coherence tomography to differentiate acquired retinoschisis from retinal detachment in difficult cases. Retina 2012;32(8):1574-1580. [PMID 22481477]
- Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol 2003;136(1):155-160. [PMID 12834683]
- Straatsma BR, Foss RY. Typical and reticular degenerative retinoschisis. Am J Ophthalmol 1973;75(4):551-575. [PMID 4572333]
- Fletcher EC, al. e. Retina: Retinoschisis. In: Cunningham ET, Riordan-Eva P, editors. Vaughan & Asbury General Ophthalmology. 18 ed. New York: McGraw-Hill; 2011; p. Ch. 10.
- Buch H, Vinding T, Nielsen NV. Prevalence and long-term natural course of retinoschisis among elderly individuals: the Copenhagen City Eye Study. Ophthalmology 2007;114(4):751-755. [PMID 17197027]
- Byer NE. Clinical study of senile retinoschisis. Arch Ophthalmol 1968;79(1):36-44. [PMID 5635087]
- Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology 1986;93(9):1127-1137. [PMID 3808625]
- Shea M, Schepens CL, Von Pirquet SR. Retionoschisis. I. Senile type: a clinical report of one hundred seven cases. Arch Ophthalmol 1960;63:1-9. [PMID 14445688]
- Byer NE. Perspectives on the management of the complications of senile retinoschisis. Eye (Lond) 2002;16(4):359-364. [PMID 12101441]
- Zimmerman LE, Spencer WH. The pathologic anatomy of retinoschisis with a report of two cases diagnosed clinically as malignant melanoma. Arch Ophthalmol 1960;63:10-19. [PMID 13847542]
- Zaidi A, Lujan B. Combined retinoschisis-detachment involving the fovea managed with observation. Retin Cases Brief Rep 2014;8(4):254-256. [PMID 25372521]
- Sneed SR, Blodi CF, Folk JC, Weingeist TA, Pulido JS. Pars plana vitrectomy in the management of retinal detachments associated with degenerative retinoschisis. Ophthalmology 1990;97(4):470-474. [PMID 2326026]
Suggested citation format:
Rice OM, Lenci LT, Sohn EH. Acquired Peripheral Retinoschisis. EyeRounds.org. October 31, 2016; Available from: https://eyerounds.org/cases/246-acquired-peripheral-retinoschisis.htm
last updated: 06/26/2017
Image Permissions:

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.
