Chief Complaint: Newly identified retinal lesion following eye exam
History of Present Illness: Patient is a 3-year-old male, initially presenting as a referral after an eye exam. The patient’s father provided the history and denied new symptoms of vision change, drifting, or crossing of the eyes. He did report noticing that the patient needed to increase the brightness level when looking at phone screens. The patient received his first pair of glasses for amblyopia two weeks prior to presentation. Since that time, the patient’s father reported good compliance with glasses. The patient has no known symptoms of hearing loss or other medical problems.
Past Ocular History: Amblyopia; treated with prescription lenses, not worn at time of visit but parents report good compliance.
Past Medical History:
Medications: None
Allergies: No known allergies
Family History:
OCULAR EXAMINATION

Chief Complaint: Newly identified retinal lesion following routine eye exam
History of Present Illness: Patient is a 4-year-old male. His initial presentation followed a failed vision screening, where the patient was instructed to start patching the left eye for possible amblyopia in the right eye. Patient’s parents report significant difficulty with patching, with behavior changes and falling asleep. At routine follow up with his local eye doctor, a retinal abnormality was noted and the patient was referred. The patient had no symptoms of hearing loss and parents did not have any specific vision concerns.
Past Ocular History: Deprivation amblyopia, right eye, attempting patching
Past Medical History:
Medications: None
Allergies: No known allergies
Family History:
OCULAR EXAMINATION
| Sphere | Cylinder | Axis | |
|---|---|---|---|
| Right | +1.75 | Sphere | |
| Left | +1.00 | +1.25 | 090 |
Chief Complaint: Newly identified retinal lesion following development of blurry vision
History of Present Illness: Patient is a 7-year-old male who was referred for newly noted retinal abnormalities identified after reporting blurry vision since start of the school year. He had also been experiencing headaches located at the back of his head that started after school, occurring several times per week. The headaches were relieved with sleep or rest and were not associated with nausea or vomiting. The patient had no history of hearing loss.
Past Ocular History: Color blindness, congenital
Past Medical History:
Medications: Mesalamine (Crohn’s disease)
Allergies: No known allergies
Family History:
OCULAR EXAMINATION
| Sphere | Cylinder | Axis | |
|---|---|---|---|
| Right | -0.50 | +0.50 | 180 |
| Left | -1.50 | +.50 | 180 |
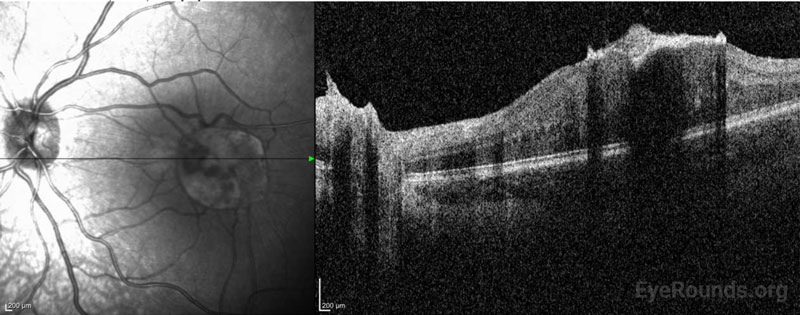
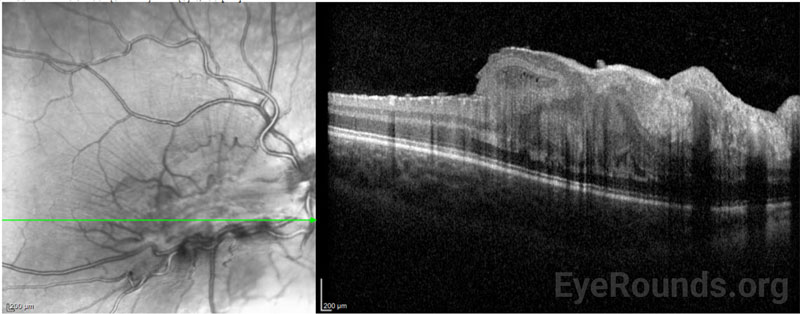
DIAGNOSIS: Combined hamartoma of the retina and retinal pigmented epithelium (CHRRPE)
CLINICAL COURSE
A diagnosis of CHRRPE was made in each of the above cases as seen on fundus photography and confirmed using OCT. There was no known family history of neurofibromatosis or associated hearing loss in any of the patients, but due to the close association of CHHRPE with neurofibromatosis type 2 (NF2), it was recommended that all patients undergo formal genetic evaluation. Two of the three described patients followed with genetics for formal genetic testing. At that time, brain and spinal MRI (Magnetic Resonance Imaging) were ordered. Normal orbits and optic nerves were appreciated in both patients and no NF2-associated lesions were observed. Additionally, there were no variants in the NF2 gene of either patient. However, a NF2 diagnosis cannot be entirely ruled out due to the possibility of mosaicism, which has been demonstrated in NF2.[1]
To date of publication, each of the described patients has remained stable. They have been evaluated every 6 months for management of amblyopia and routine counseling regarding monocular safety precautions. Patching for overlying deprivation amblyopia was attempted in each of the cases with varying degrees of success. Monocular safety precautions were strongly emphasized to each family to prevent injury to the unaffected eye.
Pars plana vitrectomy with membrane peel was deferred in each of these cases given their stability but may be considered in the future if worsening epiretinal membrane causes a decline in acuity.
DISCUSSION
Combined hamartoma of the retina and retinal pigment epithelium (CHRRPE) is a rare benign proliferation of retinal glial cells and retinal pigment epithelium (RPE) as well as vascular tissue, that distorts the retina.[3] The mean age of diagnosis is 15 years old and les.[2] It is important to distinguish CHRRPE from malignant lesions such as retinoblastoma or melanoma. Unlike choroidal melanoma, CHRRPE is uniformly pigmented and possesses clearly demarcated borders.
Although benign, the clinical manifestations of CHRRPE can include amblyopia, strabismus, vision loss, and metamorphopsia in patients.[3] Decreased vision and monocular strabismus are the most commonly reported symptoms, but as many as 2 out of 3 patients are asymptomatic at presentation.[4,5] Severity of vision loss is dependent on the location of the tumor. Macular involvement, as discussed in the associated cases, can significantly impact visual acuity (VA). CHRRPE with macular involvement have an average BCVA (best corrected visual acuity) of 20/320 compared to extramacular CHRRPE, which has an average BCVA of 20/80.
The long-term complications of CHRRPE, although rare, can include retinal detachment, vitreous and retinal hemorrhage, choroidal neovascularization, and retinoschisis.3 Routine follow-up with an ophthalmologist, protective eyewear, and amblyopia interventions are crucial for maintaining vision in the pediatric patient.
Neurofibromatosis Type 2 Association
CHRRPE can occur spontaneously and are generally unilateral in these cases. However retinal and RPE (Retinal Pigment Epithelium) tumors are strongly associated with neurofibromatosis type 2 (NF2). Neurofibromatosis type 1 (NF1) and type 2 (NF2) are phakomatoses that are characterized by tumor formation due to mutations in tumor-suppressing genes. NF2 is caused by mutations on the NF2 gene, a known tumor suppressor located on 22q12.[2] Inheritance of NF2 is typically autosomal dominant; however, de novo mutations have been documented as well as somatic mosaicism.[7,8,2]
NF2 demonstrates complete penetrance, but there is phenotypic variability. Generally, diagnosis of NF2 follows the identification of bilateral vestibular schwannomas and ocular and cutaneous tumors presenting in the 2nd and 3rd decade of life. However, pediatric patients have been identified with clinical features of NF2. In a retrospective study, the most common presenting symptom in children and young adolescents with NF2 was ophthalmic abnormalities rather than symptoms related to vestibular schwannoma as is seen in adults.[9] More specifically, studies have demonstrated retinal hamartomas in up to 22% of NF2 carriers.[7] Additional features of NF2 include meningiomas, ependymomas, and posterior subcapsular cataracts, emphasizing the importance of the ocular examination in pediatric and adult patients with NF2.
Examination and Diagnostic Testing
On dilated fundoscopic exam, CHRRPE are typically solitary and unilateral lesions that typically appear as elevated and uniformly pigmented lesions with fanlike projections. They can have different amounts of RPE, glial, and vascular components and are often usually covered by a grey-white semi-translucent membrane.1 Multimodal imaging including optical coherence tomography (OCT), standardized ocular ultrasound, and fluorescein angiography are useful in establishing a diagnosis. Additionally, serial fundus photography can help to follow the lesions over time. OCT is well tolerated by the pediatric population and can aid in diagnosis. Characteristic OCT findings in patients with CHRRPE include retinal striae, disorganization of the retina, and epiretinal membrane over the lesion surface.[10] A characteristic peak in the outer plexiform layer, referred to as a “saw tooth” pattern, is routinely described in the literature and can be observable on OCT.[11] Fundus fluorescein angiography can be used in diagnosis and to evaluate potential complications of CHRRPE such as choroidal neovascularization.12 Genetic evaluation and MRI should be considered at time of diagnosis due to the described NF2 association.
Treatment & Management
The primary goal of patching in pediatric patients with any unilateral visual threat is to prevent development of amblyopia. Amblyopia is a disruption in the eye-to-brain connection that develops when an eye is not being used due to disease or a history of trauma. It is also important for clinicians to emphasize the importance of protective eye wear, which serves as both a physical protection for the unaffected eye and a corrective lens if needed. Surgery to treat progressing ERM may be warranted in some cases. Early surgical intervention with pars plana vitrectomy with membrane peel has been shown to produce stable vision and reduce the amblyopic effect in a small study of children; however, reports of visual improvement with surgical intervention have been variable.[2] Routine follow up is necessary to evaluate for epiretinal membrane progression and neovascularization.
Differential Diagnosis:
ETIOLOGY
|
SIGNS
|
SYMPTOMS
|
MANAGEMENT
|
Gehrke E, Strampe M, Binkley E, De Andrade L. Diagnosis and Management of Combined Hamartoma of the Retina and Retinal Pigment Epithelium (CHRRPE) in Pediatric Patients. EyeRounds.org. Posted August 3, 2023; Available from https://EyeRounds.org/cases/342-chrrpe.htm

Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa are licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License.