
The University of Iowa
Department of Ophthalmology and Visual Sciences
July 13, 2017
This review covers simple optical principles of retinoscopy, describes an easily learned technique for retinoscopy with reliable results, and guides decisions based on those results through basic prescribing guidelines as they apply to children.
The estimated prevalence of refractive amblyopia varies widely by ethnic and socioeconomic groups but is estimated to be somewhere between 0.75% and 2.5% of children worldwide.[1-4] The economic impact of pediatric vision loss is difficult to estimate and is most evident only after a child reaches adulthood. However, a study from 2007 estimated 158.1 million global cases of visual impairment resulted from uncorrected or under-corrected refractive error; of these, 8.7 million were blind. This created an estimated economic productivity loss of $268.8 billion. [5]
The pediatric population with refractive error needs regular assessment and prescription adjustment due to eye growth. The cornea reaches adult size by the age of 2 years, but the eye continues to grow in anteroposterior length until age 7-8 years old. The infant eye averages 16.6 mm in anteroposterior diameter (length), and grows to an adult size averaging 22.0-24.8 mm. [6,7] Since these two variables do not have parallel growth, refractive error changes as children age.
Determining and then correcting a child's refractive error can prevent or treat amblyopia which ultimately helps to avoid irreversible vision loss. Giving children the best possible vision, including correcting refractive error when needed, allows them to succeed scholastically. Visual deficits can also affect a child's daily function and normal play which may decrease his or her confidence. Children may be unaware of less severe vision problems, particularly if anisometropia is present.
In these situations where traditional subjective refraction methods are impossible, including in young children or patients of any age with limited ability to communicate or cooperate, a method for objective refraction is required. This is also useful in cases of atypical refractive error or implausible subjective refraction results. Since retinoscopy is the gold standard for objective refraction, mastering this skill is essential.
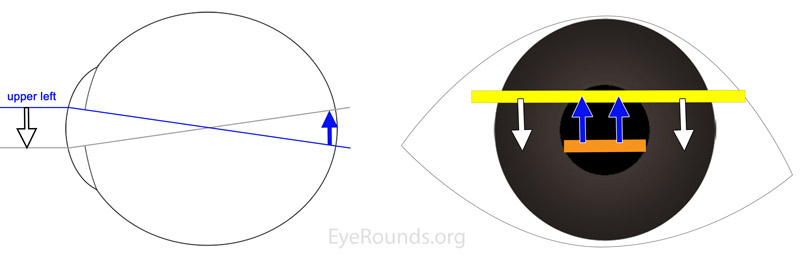
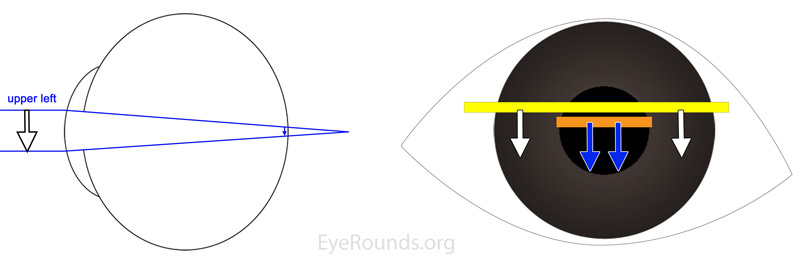
Retinoscopy allows the observer to accurately measure a patient's refractive error by determining the spherical power, cylindrical power, and cylindrical axis which focus the patient's eye at optical infinity. This is done by shining diverging light into the patient's eye from the retinoscope and finding the refraction which focuses that light on the patient's retina.
Retinoscopy results also provide information about risk factors for additional ocular morbidities. Patients with myopia have higher rates of other significant ocular disease, such as retinal detachment and glaucoma.[8,9] Patients with severe hyperopia are more likely to develop accommodative esotropia (see "Special Considerations for Spectacles in Children" section) and amblyopia.[10] A subgroup of children with crowded anterior segment and high hyperopia have an increased risk of angle closure glaucoma.
There are a few valuable trends to keep in mind when determining refractive error and prescribing spectacles for children. First, refractive error typically moves from hyperopia toward myopia as children age. Roughly 80% of children between 2 and 6 years old are hyperopic and about 10% of children need refractive correction before 8 years old.[11] Myopia then develops between 6 – 9 years old and frequently increases throughout adolescence.[11] Second, astigmatism is relatively common in babies but decreases in prevalence during the first few years of life.[11] The newborn eye averages a K value (diopters) of 51.2, while the adult eye averages a K value of 43.5 diopters.[12] Thus, although the focusing power of the eye decreases with age, there is a simultaneous trend away from hyperopia -- meaning the eye needs less additional corrective power -- because of simultaneous axial eye length increase as the patient ages.
Multiple methods of retinoscopy exist and have been extensively described. Here we aim to simply describe the basic concept and specifically one common method: plus cylinder neutralization retinoscopy. Please refer to other resources for a more exhaustive description of additional techniques and their applications.



The examiner should place himself aligned with the pupil while the patient is looking at a distant object. The examiner then obtains a red reflex with a "streak" of light and passes that streak of light perpendicular to the axis of the streak. By observing the pattern of "with" or "against" motion, the examiner can interchange a lens with more plus power or less plus power to the point where the retinoscopic reflex is "neutralized." At this point, instead of moving against or with the movement of the streak, the reflex will appear as a diffuse, even light that changes very little as the examiner moves the retinoscope. For plus-cylinder refractions, the examiner starts by neutralizing the meridian with the lower hyperopic power, thereby leaving the meridian 90 degrees away with "with motion." The examiner then neutralizes this second meridian, noting the axis, and calculates the power difference between the two lenses needed for neutralization (plus cylinder power). The examiner then "takes out the working distance" from the lowest hyperopic power which gives the final spherical refraction.
Once a child's refractive error has been determined, the next decision is whether or not to prescribe corrective lenses. When a child is less than 9 years old, considerations include whether the refractive error is normal for a child's age, and whether the uncorrected error will cause amblyopia or interfere with the child's visual function and alignment. Whether wearing corrective lenses will interfere with emmetropization is controversial. Some providers will prescribe a little less power than needed to encourage emmetropization of the eye, perhaps because the rate of emmetropization is related to the total initial refractive error in infants.[13] A recent study found that prescribing the smallest amount of hyperopic correction needed to allow near-focusing does not impede emmetropization.[14] In daily practice, for hyperopic patients, lower than full plus prescription seems to be better tolerated and accepted by children except in cases of accommodative esotropia, where the full cycloplegic correction is necessary to minimize or eliminate strabismus.
The following guidelines come from the American Academy of Ophthalmology's preferred practice patterns. These guidelines represent the minimum values at which spectacle prescription is recommended for isolated refractive error, specifically in the absence of amblyopia or strabismus which should lower the threshold for spectacle prescription.
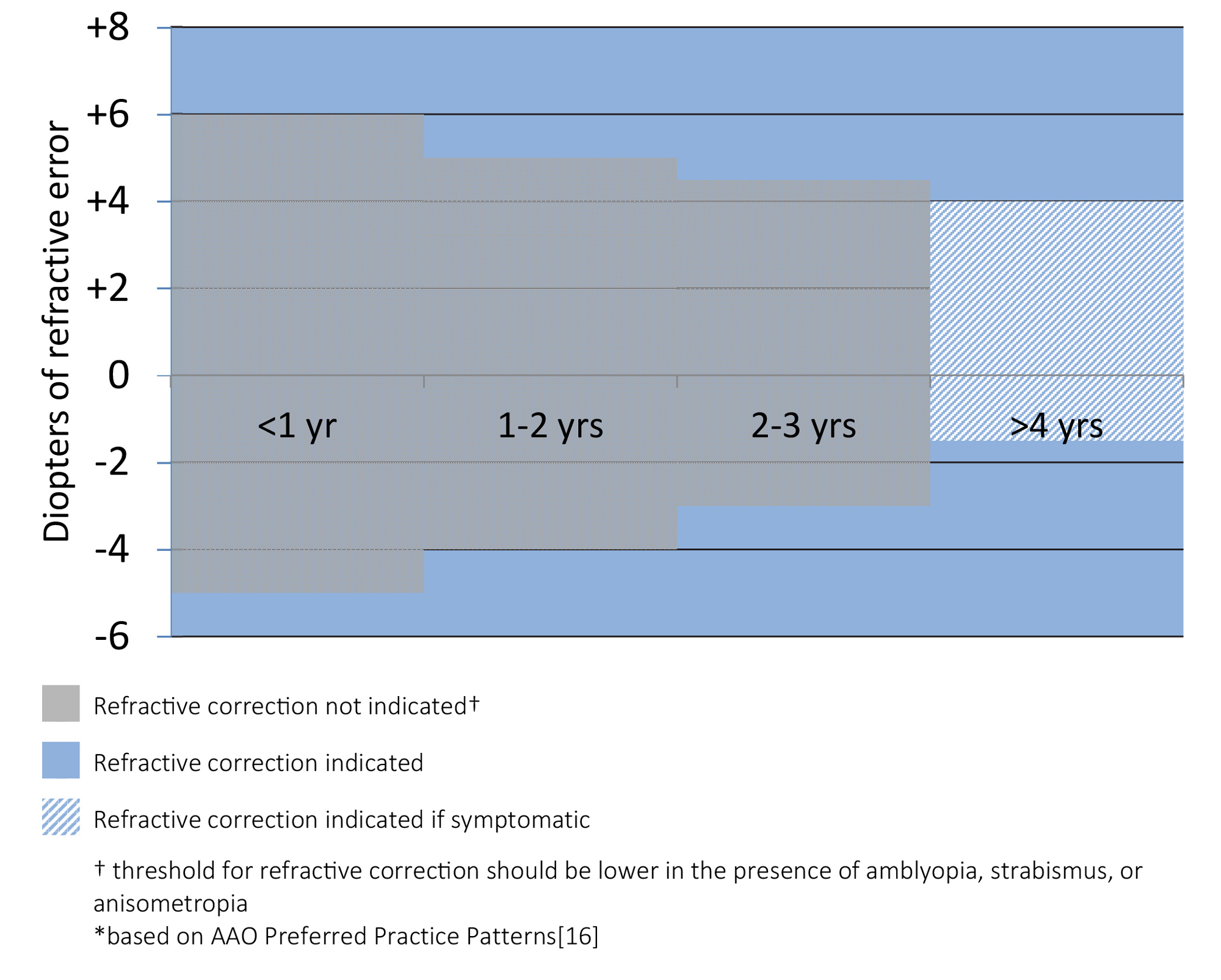
Prescribe anisometric difference at any age if amblyopia is present
Lens power may be reduced ("minus lens therapy") from the cycloplegic refraction, even for minor prescriptions, to induce accommodative convergence and reduce exotropia.[18]
Prescribe the full amount of correction with +2 to +3 D (retinoscopy will show -2 to -3D) to allow near activities, since infants are primarily interested in objects near them. At around 1.5-2 years of age, bifocals can be considered.
Correct the full anisometropia, astigmatism, and myopia to cycloplegic refraction. Correct hyperopia that is >3 D to either full cycloplegic refraction, or to a level that is under corrected by as much as 1.5 D. Using this prescribing guideline (without the need for occlusion therapy or other therapies) has been shown to resolve anisometropic amblyopia in roughly one third of cases..10-21]
Evans J, Risma T, Dumitrescu A. Pediatric Spectacle Prescription and Retinoscopy Made Simple. EyeRounds.org. posted July 13, 2017; Available from: https://eyerounds.org/tutorials/pediatric-spectacle-prescription-and-retinoscopy/