
Section 3-A: Normal Ocular Anatomy
A brief review of the normal anatomy and function of the eye will serve as a basis for understanding the abnormal disease processes that cause glaucoma.
Many of the structures of the eye closely resemble the components of a camera (Figure 3-1). The cornea and the lens focus images on the retina and are similar to the lens of a camera. The retina is the tissue of the eye that senses light and functions like the film of a camera. The iris controls the amount of the light that enters the eye as the diaphragm on a camera lens regulates the amount of light passing into the camera. Finally, the images detected by the retina are delivered by the optic nerve to the brain where vision is perceived. The optic nerve is the part of the eye that is damaged by glaucoma.
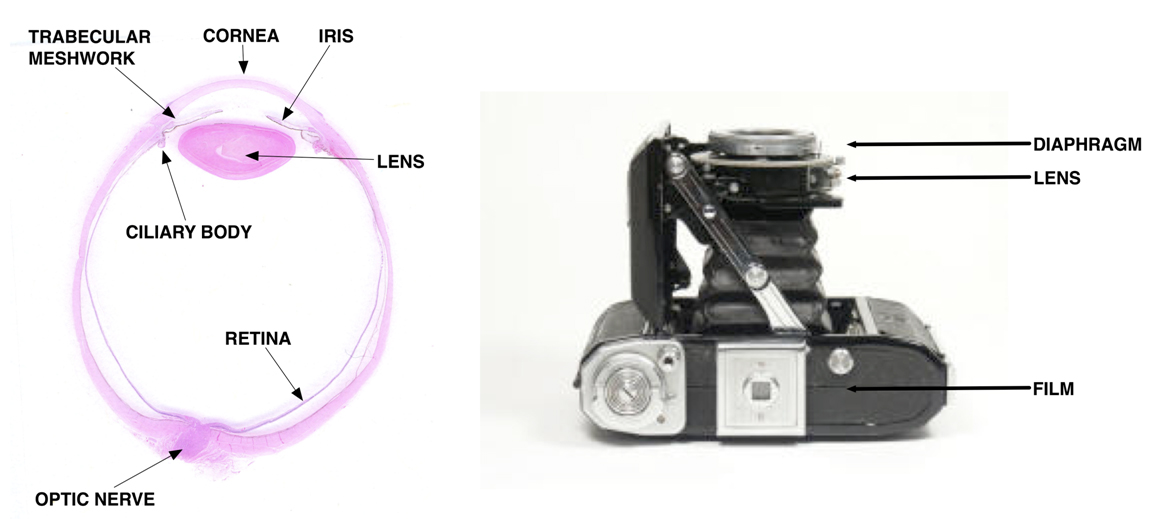
Figure 3-1. Structures of the eye are indicated on the cross-sectional image of a human eye shown on the left and a camera is shown on the right for comparison. (The image of the eye is courtesy of Nasreen Syed, MD, University of Iowa).
Section 3-B: Aqueous fluid production and drainage angle.
The cornea and the lens have no blood supply. They receive nourishment from nutrients in the aqueous fluid that fills the eye. The aqueous fluid is produced by the ciliary body, which is located behind the iris (Figure 3-2). The aqueous fluid enters the eye through the ciliary body and flows between the iris and lens through the pupil. The fluid passes out of the eye through a tissue called the trabecular meshwork, which is at the drainage angle (at the junction of the cornea and the iris). As the aqueous fluid passes through the eye, it supplies the lens and cornea with nutrients and carries away waste products.
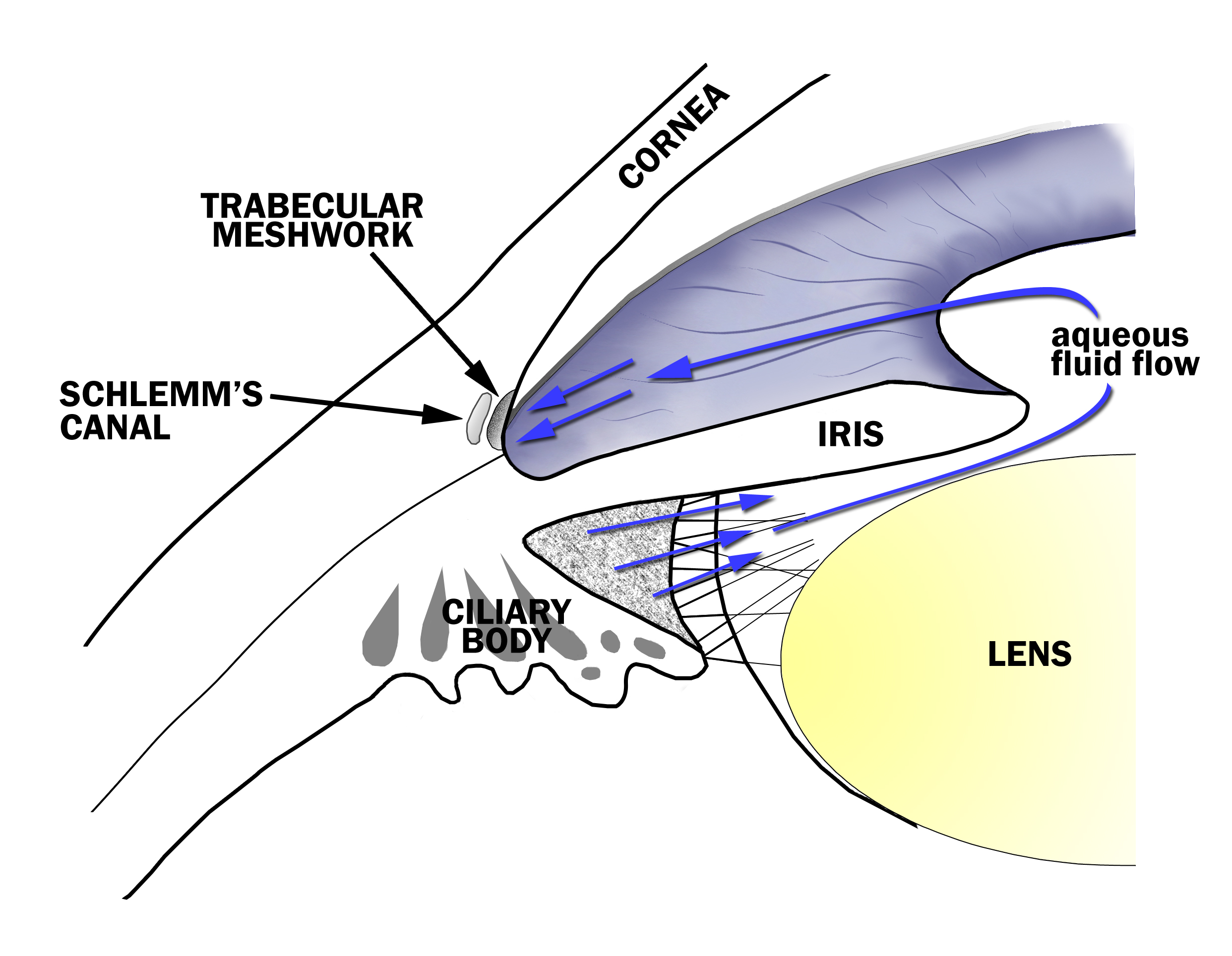
Figure 3-2. Aqueous Fluid Flow in the Eye. The aqueous fluid that fills the eye is produced by the ciliary body and flows between the iris and lens, through the pupil and to the drainage angle at the junction of the iris and the cornea. Aqueous fluid exits the eye through a tissue called the trabecular meshwork in the drainage angle.
The pressure of the fluid in the eye (intraocular pressure) is determined by the amount of fluid entering the eye through the ciliary body and exiting the eye through the trabecular meshwork. In most people, the balance between the fluid coming in and going out of the eye results in an eye pressure between 10 and 21 mm of Hg. In patients with glaucoma, fluid drains from the eye through the trabecular meshwork at a slower rate causing the pressure in the eye to rise.
Eye doctors regularly examine the drainage angle to see if there is any visible obstruction to fluid leaving the eye through the trabecular meshwork. A special lens (gonioscopy lens) is needed to examine the trabecular meshwork (Figure 3-3A – 3-3B). The gonioscopy lens is gently placed against the surface of the cornea and allows eye doctors to see the trabecular meshwork in the drainage angle (Figure 3-3C).
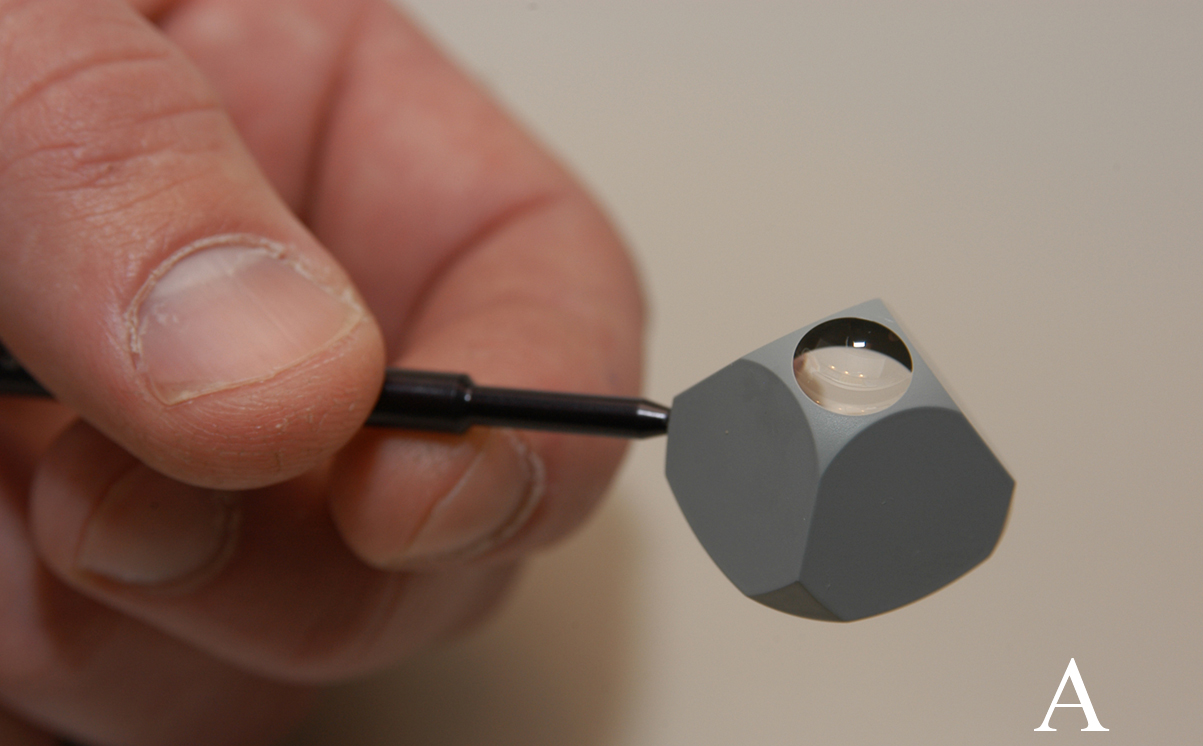
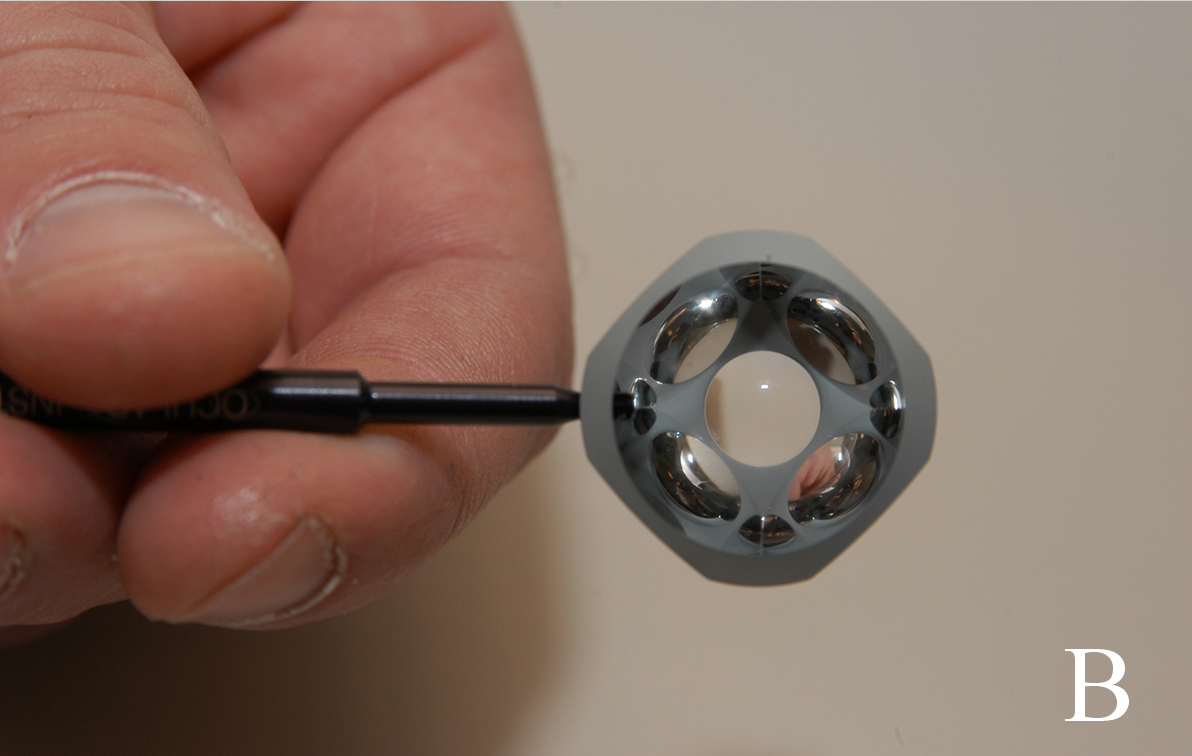
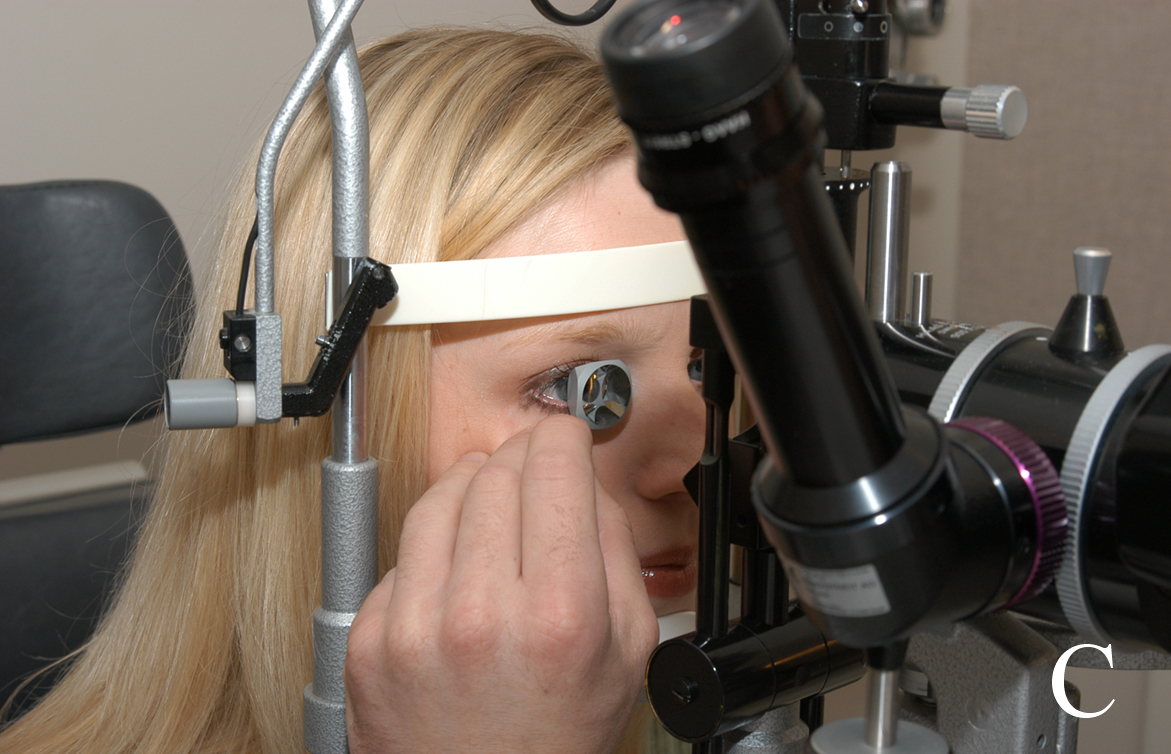
Figure 3-3. Gonioscopy. A and B The drainage angle is examined using a special lens (gonioscopy lens). C. The gonioscopy lens is gently held against the cornea. Eye doctors look through the gonioscopy lens to see the drainage angle.
There are two major types of glaucoma. In open-angle glaucoma, the drainage angle between the cornea and the iris is wide open and allows the aqueous fluid of the eye to make its way to the trabecular meshwork – the chief site for fluid drainage from the eye. In patients with open-angle glaucoma, (non-visible) abnormalities in the trabecular meshwork reduce the outflow of aqueous humor. In angle closure glaucoma the trabecular meshwork is visibly obstructed and the aqueous humor is prevented from draining out of the eye.
Section 3-C: Optic nerve damage.
The primary function of the optic nerve is to convey visual signals received by the retina to the brain. As described in Chapter 1, specific sections of the optic nerve are responsible for transmitting particular parts of the visual field to the brain. If part of the optic nerve is damaged by glaucoma, the visual signals from a portion of the visual field are no longer reported to the brain and a blind-spot (called scotoma) is formed.
Eye doctors may directly observe damage to the optic nerve damage by looking through the pupil with an ophthalmoscope. A healthy optic nerve is pink, and the ratio of the diameter of the optic cup to that of the optic disc in a healthy eye is generally less than 0.5 (see Chapter 1-B for more discussion). When the optic nerve is damaged many of the individual fibers that make up the nerve are lost and the optic nerve becomes excavated or “cupped.” As glaucoma progresses and more optic nerve tissue is lost, the optic cup grows larger (Figure 3-4).
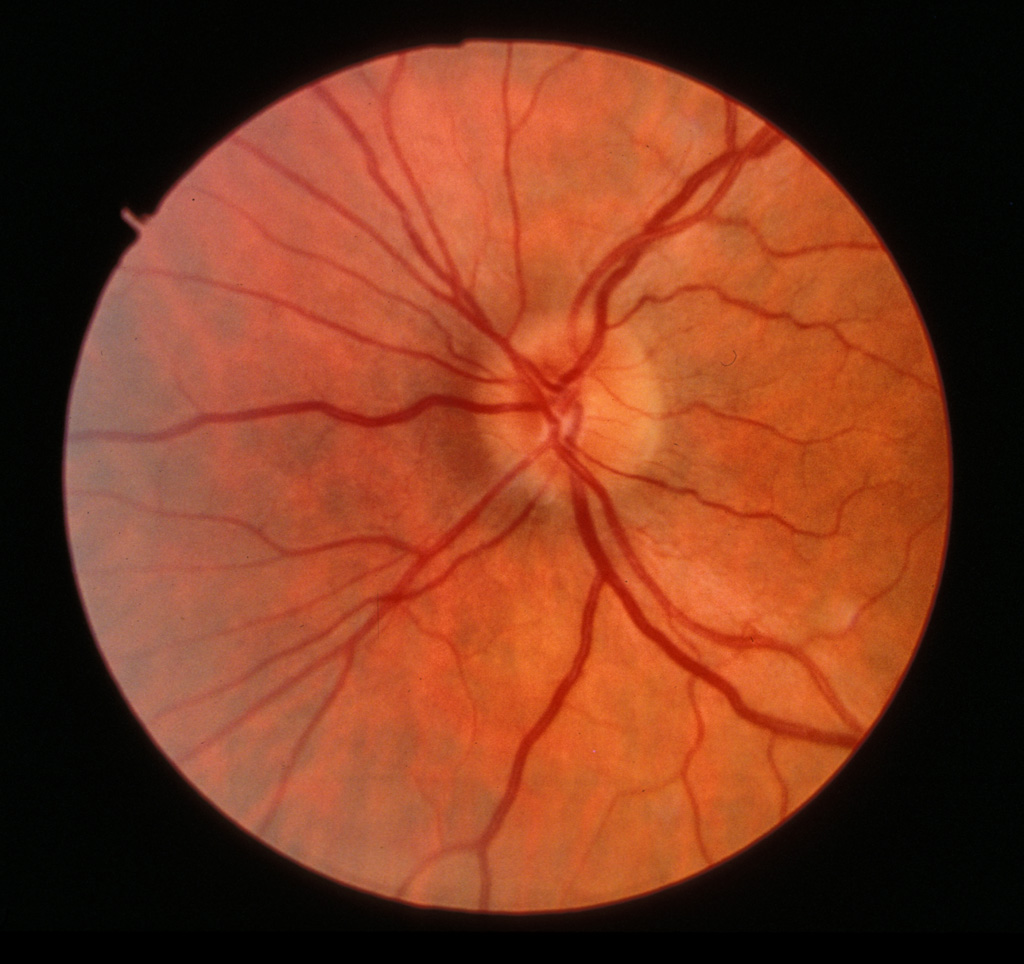
Figure 3-4A. Optic cup which was initially not visible
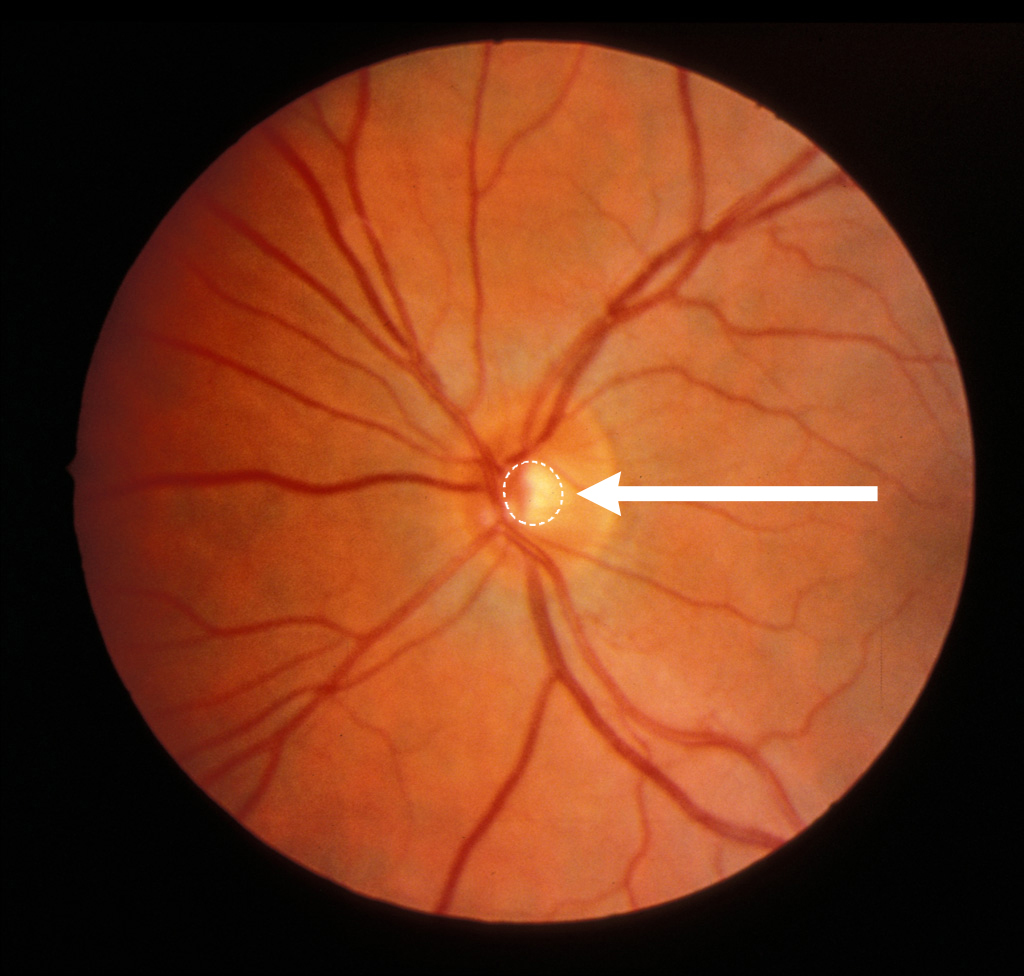
Figure 3-4B. Enlarged optic cup over time
Figure 3-4. Progressive cupping of the optic disc. Open and closed drainage angles. Early progression of cupping can be seen by comparing sequential photographs of the optic nerve. The optic cup which was initially not visible (A) has enlarged over time (B).
The superior and inferior aspects of the optic nerve are preferentially damaged by glaucoma. These parts of the nerve are responsible for peripheral vision. Consequently, as the optic cup enlarges, it typically becomes vertically elongated. In advanced stages of glaucoma the portion of the nerve that carries central vision may also become involved.
Bleeding or hemorrhage of the optic nerve is another sign of damage from glaucoma. There is a characteristic appearance to optic nerve hemorrhage that is due to the anatomy of the eye. When the optic nerve bleeds in glaucoma, the blood typically collects along the individual nerve fibers that radiate outwards from the nerve (Figure 3-5.) An optic nerve hemorrhage is a sign that glaucoma may not be under good control, and additional therapy may be necessary to bring the glaucoma under control.
The cause of the optic nerve damage in glaucoma is not well understood. In some patients that have elevated intraocular pressure, the progression of glaucoma is halted when the pressure is lowered to a more normal level with medicines or surgery. High intraocular pressure may directly damage the optic nerve and cause disease in this subset of patients. In other patients, the optic nerve is injured at pressures that are not elevated (or in the normal range). The optic nerves of these patients (so-called “normal tension glaucoma” patients) appear to be sensitive to damage at intraocular pressures that most people tolerate without any harmful effects. Studies have shown that lowering the intraocular pressure to low normal or even sub-normal levels can halt the progression of normal tension glaucoma. Additional mechanisms such as poor blood circulation to the optic nerve may be responsible for optic nerve damage in normal tension glaucoma.
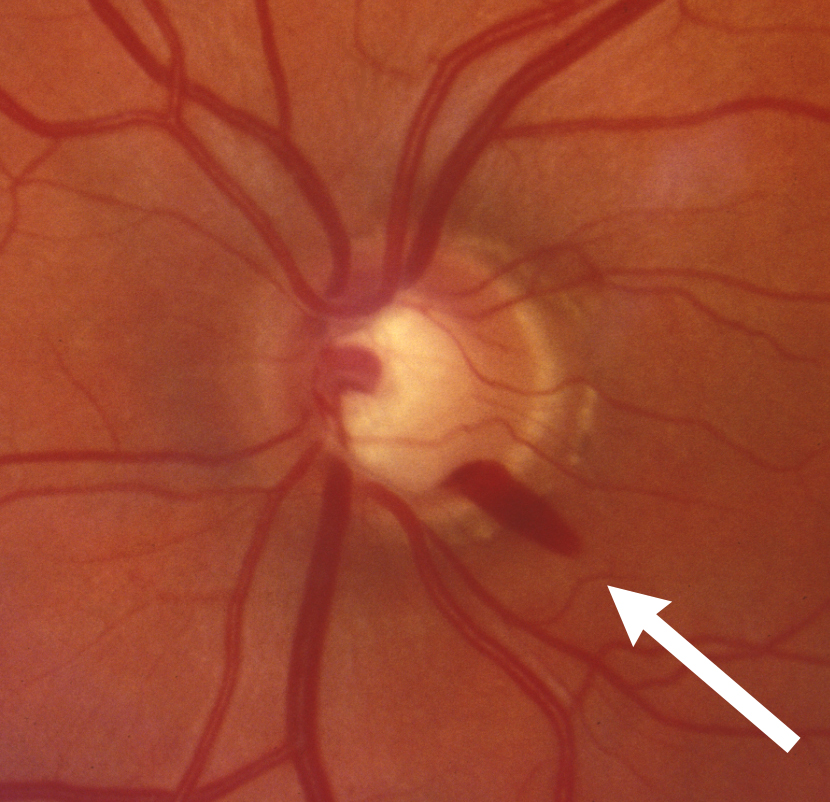
Figure 3-5. Optic nerve hemorrhage. There is a flame-shaped hemorrhage of the optic nerve located at the arrow at 5 o’clock
Chapter 3. References
Alward, WLM. Aqueous system anatomy and physiology. In Glaucoma: The Requisites in Ophthalmology. JH Krachmer (ed.) Saint Louis: Mosby, Chapter 2, 2000.
Anderson, DR. Collaborative Normal Tension Glaucoma Study. Current Opinion in Ophthalmology. 14: 86-90.
Millar, JC, Gabert, BT, Kaufman, PL. Aqueous Humor Dynamics. In Duane’s Clinical Ophthalmology. W Tasman and EA Jaeger (eds.) Saint Louis: Lippincott Williams & Wilkins, Chapter 45, 2005.